Bacterial vaginosis (BV) is an infection of the vagina caused by excessive growth of bacteria. Common symptoms include increased vaginal discharge that often smells like fish. The discharge is usually white or gray in color. Burning with urination may occur. Itching is uncommon. Occasionally, there may be no symptoms. Having BV approximately doubles the risk of infection by a number of sexually transmitted infections, including HIV/AIDS. It also increases the risk of early delivery among pregnant women.

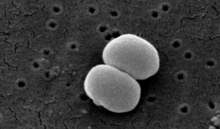
Candidiasis is a fungal infection due to any species of the genus Candida. When it affects the mouth, in some countries it is commonly called thrush. Signs and symptoms include white patches on the tongue or other areas of the mouth and throat. Other symptoms may include soreness and problems swallowing. When it affects the vagina, it may be referred to as a yeast infection or thrush. Signs and symptoms include genital itching, burning, and sometimes a white "cottage cheese-like" discharge from the vagina. Yeast infections of the penis are less common and typically present with an itchy rash. Very rarely, yeast infections may become invasive, spreading to other parts of the body. This may result in fevers along with other symptoms depending on the parts involved.

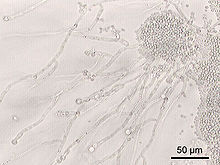
Lactobacillus is a genus of gram-positive, aerotolerant anaerobes or microaerophilic, rod-shaped, non-spore-forming bacteria. Until 2020, the genus Lactobacillus comprised over 260 phylogenetically, ecologically, and metabolically diverse species; a taxonomic revision of the genus assigned lactobacilli to 25 genera.

The human microbiome is the aggregate of all microbiota that reside on or within human tissues and biofluids along with the corresponding anatomical sites in which they reside, including the skin, mammary glands, seminal fluid, uterus, ovarian follicles, lung, saliva, oral mucosa, conjunctiva, biliary tract, and gastrointestinal tract. Types of human microbiota include bacteria, archaea, fungi, protists, and viruses. Though micro-animals can also live on the human body, they are typically excluded from this definition. In the context of genomics, the term human microbiome is sometimes used to refer to the collective genomes of resident microorganisms; however, the term human metagenome has the same meaning.
Vaginitis, also known as vulvovaginitis, is inflammation of the vagina and vulva. Symptoms may include itching, burning, pain, discharge, and a bad smell. Certain types of vaginitis may result in complications during pregnancy.

Lactobacillus acidophilus is a rod-shaped, Gram-positive, homofermentative, anaerobic microbe first isolated from infant feces in the year 1900. The species is most commonly found in humans, specifically the gastrointestinal tract, oral cavity, and vagina, as well as various fermented foods such as fermented milk or yogurt. The species most readily grows at low pH levels, and has an optimum growth temperature of 37 °C. Certain strains of L. acidophilus show strong probiotic effects, and are commercially used in dairy production. The genome of L. acidophilus has been sequenced.

Vaginal discharge is a mixture of liquid, cells, and bacteria that lubricate and protect the vagina. This mixture is constantly produced by the cells of the vagina and cervix, and it exits the body through the vaginal opening. The composition, amount, and quality of discharge varies between individuals and can vary throughout the menstrual cycle and throughout the stages of sexual and reproductive development. Normal vaginal discharge may have a thin, watery consistency or a thick, sticky consistency, and it may be clear or white in color. Normal vaginal discharge may be large in volume but typically does not have a strong odor, nor is it typically associated with itching or pain. While most discharge is considered physiologic or represents normal functioning of the body, some changes in discharge can reflect infection or other pathological processes. Infections that may cause changes in vaginal discharge include vaginal yeast infections, bacterial vaginosis, and sexually transmitted infections. The characteristics of abnormal vaginal discharge vary depending on the cause, but common features include a change in color, a foul odor, and associated symptoms such as itching, burning, pelvic pain, or pain during sexual intercourse.

Aposymbiosis occurs when symbiotic organisms live apart from one another. Studies have shown that the lifecycles of both the host and the symbiont are affected in some way, usually negative, and that for obligate symbiosis the effects can be drastic. Aposymbiosis is distinct from exsymbiosis, which occurs when organisms are recently separated from a symbiotic association. Because symbionts can be vertically transmitted from parent to offspring or horizontally transmitted from the environment, the presence of an aposymbiotic state suggests that transmission of the symbiont is horizontal. A classical example of a symbiotic relationship with an aposymbiotic state is the Hawaiian bobtail squid Euprymna scolopes and the bioluminescent bacteria Vibrio fischeri. While the nocturnal squid hunts, the bacteria emit light of similar intensity of the moon which camouflages the squid from predators. Juveniles are colonized within hours of hatching and Vibrio must outcompete other bacteria in the seawater through a system of recognition and infection.
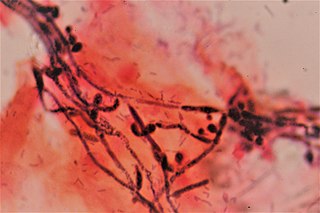
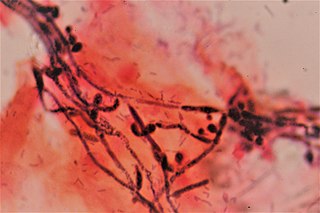
Dysbiosis is characterized by a disruption to the microbiome resulting in an imbalance in the microbiota, changes in their functional composition and metabolic activities, or a shift in their local distribution. For example, a part of the human microbiota such as the skin flora, gut flora, or vaginal flora, can become deranged, with normally dominating species underrepresented and normally outcompeted or contained species increasing to fill the void. Dysbiosis is most commonly reported as a condition in the gastrointestinal tract.

Vaginal flora, vaginal microbiota or vaginal microbiome are the microorganisms that colonize the vagina. They were discovered by the German gynecologist Albert Döderlein in 1892 and are part of the overall human flora. The amount and type of bacteria present have significant implications for an individual's overall health. The primary colonizing bacteria of a healthy individual are of the genus Lactobacillus, such as L. crispatus, and the lactic acid they produce is thought to protect against infection by pathogenic species.
Prevotella is a genus of Gram-negative bacteria.
Tannerella forsythia is an anaerobic, Gram-negative bacterial species of the Bacteroidota phylum. It has been implicated in periodontal diseases and is a member of the red complex of periodontal pathogens. T. forsythia was previously named Bacteroides forsythus and Tannerella forsythensis.
Vaginal yeast infection, also known as candidal vulvovaginitis and vaginal thrush, is excessive growth of yeast in the vagina that results in irritation. The most common symptom is vaginal itching, which may be severe. Other symptoms include burning with urination, a thick, white vaginal discharge that typically does not smell bad, pain during sex, and redness around the vagina. Symptoms often worsen just before a woman's period.
The vaginal flora in pregnancy, or vaginal microbiota in pregnancy, is different from the vaginal flora before sexual maturity, during reproductive years, and after menopause. A description of the vaginal flora of pregnant women who are immunocompromised is not covered in this article. The composition of the vaginal flora significantly differs in pregnancy. Bacteria or viruses that are infectious most often have no symptoms.
Lactobacillus jensenii is a normal inhabitant of the lower reproductive tract in healthy women. L. jensenii makes up 23% of vaginal microflora that is naturally occurring. It is also found on the skins of grapes at the time of their harvest. L. jensenii is sometimes used in producing fermented foods.

The placental microbiome is the nonpathogenic, commensal bacteria claimed to be present in a healthy human placenta and is distinct from bacteria that cause infection and preterm birth in chorioamnionitis. Until recently, the healthy placenta was considered to be a sterile organ but now genera and species have been identified that reside in the basal layer.

The uterine microbiome is the commensal, nonpathogenic, bacteria, viruses, yeasts/fungi present in a healthy uterus, amniotic fluid and endometrium and the specific environment which they inhabit. It has been only recently confirmed that the uterus and its tissues are not sterile. Due to improved 16S rRNA gene sequencing techniques, detection of bacteria that are present in low numbers is possible. Using this procedure that allows the detection of bacteria that cannot be cultured outside the body, studies of microbiota present in the uterus are expected to increase.
LACTIN-V, also known as CTV-05 or as Lactobacillus crispatus CTV-05, is a live biopharmaceutical medication containing a strain of Lactobacillus crispatus (L. crispatus) which is under development for the treatment of urinary tract infections (UTIs) and bacterial vaginosis (BV). It is administered intravaginally and is described as the first vaginal microbiome (VMB)-based live biotherapeutic product (LBP). Depletion of hydrogen peroxide (H2O2)-producing Lactobacillus strains such as Lactobacillus crispatus in the vagina has been strongly associated with BV and UTIs. Most commercially available probiotic Lactobacillus strains are not vaginal strains and do not appear to improve vaginal or urinary health outcomes. The Centers for Disease Control and Prevention (CDC)'s Sexually Transmitted Infections Treatment Guidelines (2021) noted that intravaginal LACTIN-V produced a considerably lower recurrence of BV following initial antibiotic treatment with metronidazole in a randomized controlled trial. However, the guidelines also noted that LACTIN-V is not yet Food and Drug Administration (FDA)-approved or commercially available. As of December 2021, LACTIN-V is in phase 2/3 clinical trials for the treatment of UTIs and is in phase 2 trials for the treatment of BV. It was originated by GyneLogix and is under development by Osel Inc., the National Institute of Allergy and Infectious Diseases, and other organizations.