Gender dysphoria (GD) is the distress a person experiences due to a mismatch between their gender identity—their personal sense of their own gender—and their sex assigned at birth. The term replaced the previous diagnostic label of gender identity disorder (GID) in 2013 with the release of the diagnostic manual DSM-5. The condition was renamed to remove the stigma associated with the term disorder.
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender. The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals. It is also known as sex reassignment surgery, gender confirmation surgery, and several other names.
The World Professional Association for Transgender Health (WPATH), formerly the Harry Benjamin International Gender Dysphoria Association (HBIGDA), is a professional organization devoted to the understanding and treatment of gender identity and gender dysphoria, and creating standardized treatment for transgender and gender variant people. WPATH was founded in September 1979 by endocrinologist and sexologist Harry Benjamin, with the goal of creating an international community of professionals specializing in treating gender variance.
The Standards of Care for the Health of Transgender and Gender Diverse People (SOC) is an international clinical protocol by the World Professional Association for Transgender Health (WPATH) outlining the recommended assessment and treatment for transgender and gender-diverse individuals across the lifespan including social, hormonal, or surgical transition. It often influences clinicians' decisions regarding patients' treatment. While other standards, protocols, and guidelines exist – especially outside the United States – the WPATH SOC is the most widespread protocol used by professionals working with transgender or gender-variant people.
Gender transition is the process of affirming and expressing one's internal sense of gender, as opposed to the gender assigned to them at birth. There are two major facets of gender transitioning: a social transition, and a medical transition; almost all transgender people will socially transition, and most will undergo some degree of medical transition.
Pediatric endocrinology is a medical subspecialty dealing with disorders of the endocrine glands, such as variations of physical growth and sexual development in childhood, diabetes and many more.

Triptorelin, sold under the brand name Decapeptyl among others, is a medication that acts as an agonist analog of gonadotropin-releasing hormone, repressing expression of luteinizing hormone (LH) and follicle-stimulating hormone (FSH).

Gonadotropin-releasing hormone antagonists are a class of medications that antagonize the gonadotropin-releasing hormone receptor and thus the action of gonadotropin-releasing hormone (GnRH). They are used in the treatment of prostate cancer, endometriosis, uterine fibroids, female infertility in assisted reproduction, and for other indications.
Gender dysphoria in children (GD), also known as gender incongruence of childhood, is a formal diagnosis for children who experience significant discontent due to a mismatch between their assigned sex and gender identity. The diagnostic label gender identity disorder in children (GIDC) was used by the Diagnostic and Statistical Manual of Mental Disorders (DSM) until it was renamed gender dysphoria in children in 2013 with the release of the DSM-5. The diagnosis was renamed to remove the stigma associated with the term disorder.
Gender incongruence is the state of having a gender identity that does not correspond to one's sex assigned at birth. This is experienced by people who identify as transgender or transsexual, and often results in gender dysphoria. The causes of gender incongruence have been studied for decades.
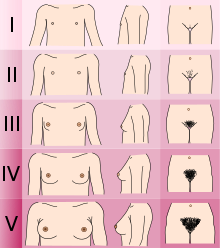
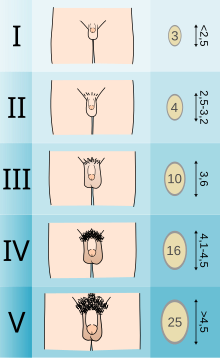
Masculinizing hormone therapy, also known as transmasculine hormone therapy or female-to-male hormone therapy, is a form of hormone therapy and gender affirming therapy which is used to change the secondary sexual characteristics of transgender people from feminine or androgynous to masculine. It is a common type of transgender hormone therapy, and is predominantly used to treat transgender men and other transmasculine individuals who were assigned female at birth. Some intersex people also receive this form of therapy, either starting in childhood to confirm the assigned sex or later if the assignment proves to be incorrect.
Feminizing hormone therapy, also known as transfeminine hormone therapy, is hormone therapy and sex reassignment therapy to change the secondary sex characteristics of transgender people from masculine or androgynous to feminine. It is a common type of transgender hormone therapy and is used to treat transgender women and non-binary transfeminine individuals. Some, in particular intersex people, but also some non-transgender people, take this form of therapy according to their personal needs and preferences.

A transsexual person is someone who experiences a gender identity that is inconsistent with their assigned sex, and desires to permanently transition to the sex or gender with which they identify, usually seeking medical assistance to help them align their body with their identified sex or gender.

A trans woman is a woman who was assigned male at birth. Trans women have a female gender identity and may experience gender dysphoria. Gender dysphoria may be treated with gender-affirming care.

Cyproterone acetate (CPA), sold alone under the brand name Androcur or with ethinylestradiol under the brand names Diane or Diane-35 among others, is an antiandrogen and progestin medication used in the treatment of androgen-dependent conditions such as acne, excessive body hair growth, early puberty, and prostate cancer, as a component of feminizing hormone therapy for transgender individuals, and in birth control pills. It is formulated and used both alone and in combination with an estrogen. CPA is taken by mouth one to three times per day.
Puberty blockers are medicines used to postpone puberty in children. The most commonly used puberty blockers are gonadotropin-releasing hormone (GnRH) agonists, which suppress the natural production of sex hormones, such as androgens and estrogens. Puberty blockers are used to delay the development of unwanted secondary sex characteristics in transgender children, so as to allow transgender youth more time to explore their gender identity. The same drugs are also used to treat other conditions, such as precocious puberty in young children and some hormone-sensitive cancers in adults.
The real-life experience (RLE), sometimes called the real-life test (RLT), is a period of time or process in which transgender individuals live full-time in their identified gender role in order to be eligible to receive gender-affirming treatment. The purpose of the RLE has been to confirm that a given transgender person could function successfully as a member of said gender in society, as well as to confirm that they are sure they want to live as said gender for the rest of their life. A documented RLE was previously a requirement of many physicians before prescribing gender-affirming hormone therapy, and a requirement of most surgeons before performing gender-affirming surgery.
Transgender pregnancy is the gestation of one or more embryos or fetuses by transgender people. As of 2024, the possibility is restricted to those born with female reproductive systems. However, transition-related treatments may impact fertility. Transgender men and nonbinary people who are or wish to become pregnant face social, medical, legal, and psychological concerns. As uterus transplantations are currently experimental, and none have successfully been performed on trans women, they cannot become pregnant.
Transgender health care includes the prevention, diagnosis and treatment of physical and mental health conditions for transgender individuals. A major component of transgender health care is gender-affirming care, the medical aspect of gender transition. Questions implicated in transgender health care include gender variance, sex reassignment therapy, health risks, and access to healthcare for trans people in different countries around the world. Gender affirming health care can include psychological, medical, physical, and social behavioral care. The purpose of gender affirming care is to help a transgender individual conform to their desired gender identity.
The medical uses of bicalutamide, a nonsteroidal antiandrogen (NSAA), include the treatment of androgen-dependent conditions and hormone therapy to block the effects of androgens. Indications for bicalutamide include the treatment of prostate cancer in men, skin and hair conditions such as acne, seborrhea, hirsutism, and pattern hair loss in women, high testosterone levels in women, hormone therapy in transgender women, as a puberty blocker to prevent puberty in transgender girls and to treat early puberty in boys, and the treatment of long-lasting erections in men. It may also have some value in the treatment of paraphilias and hypersexuality in men.