Nicotine is a chiral alkaloid that is naturally produced in the nightshade family of plants and is widely used as a stimulant. As a pharmaceutical drug, it is used for smoking cessation to relieve withdrawal symptoms. Nicotine acts as a receptor agonist at most nicotinic acetylcholine receptors (nAChRs), except at two nicotinic receptor subunits where it acts as a receptor antagonist.

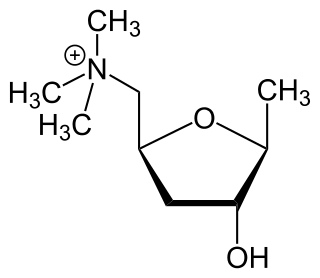
Acetylcholine (ACh) is an organic chemical that functions in the brain and body of many types of animals as a neurotransmitter—a chemical message released by nerve cells to send signals to other cells, such as neurons, muscle cells and gland cells. Its name is derived from its chemical structure: it is an ester of acetic acid and choline. Parts in the body that use or are affected by acetylcholine are referred to as cholinergic. Substances that increase or decrease the overall activity of the cholinergic system are called cholinergics and anticholinergics, respectively.

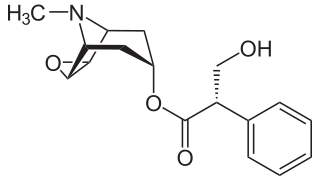
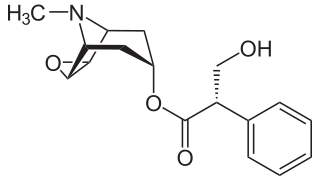
Atropine is a medication used to treat certain types of nerve agent and pesticide poisonings as well as some types of slow heart rate, and to decrease saliva production during surgery. It is typically given intravenously or by injection into a muscle. Eye drops are also available which are used to treat uveitis and early amblyopia. The intravenous solution usually begins working within a minute and lasts half an hour to an hour. Large doses may be required to treat some poisonings.

Benzatropine (INN), known as benztropine in the United States and Japan, is a medication used to treat a type of movement disorder due to antipsychotics known as dystonia and parkinsonism. It is not useful for tardive dyskinesia. It is taken by mouth or by injection into a vein or muscle. Benefits are seen within two hours and last for up to ten hours.

Atropa belladonna, commonly known as belladonna or deadly nightshade, is a poisonous perennial herbaceous plant in the nightshade family Solanaceae, which also includes tomatoes, potatoes, and eggplant (aubergine). It is native to Europe, North Africa, and Western Asia. Its distribution extends from Great Britain in the west to western Ukraine and the Iranian province of Gilan in the east. It is also naturalised or introduced in some parts of Canada and the United States.

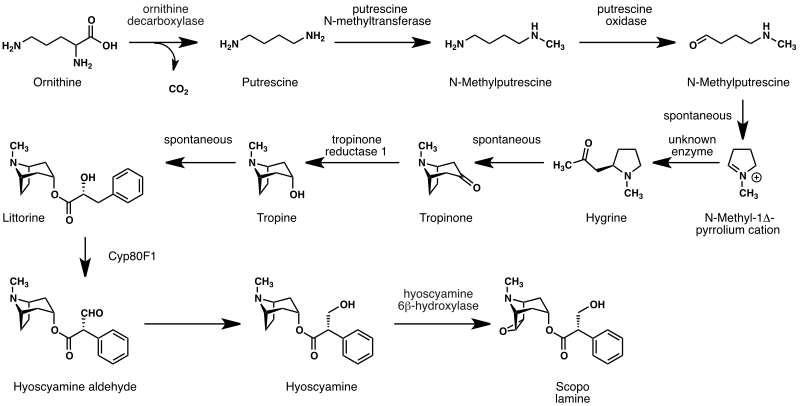
Hyoscyamine is a naturally occurring tropane alkaloid and plant toxin. It is a secondary metabolite found in certain plants of the family Solanaceae, including henbane, mandrake, angel's trumpets, jimsonweed, tomato, the sorcerers' tree, and deadly nightshade. It is the levorotary isomer of atropine and thus sometimes known as levo-atropine.
Anticholinergics are a group of substances that blocks the action of the neurotransmitter called acetylcholine (ACh) at synapses in the central and peripheral nervous system.

Chlorphenamine, also known as chlorpheniramine, is an antihistamine used to treat the symptoms of allergic conditions such as allergic rhinitis. It is taken by mouth. The medication takes effect within 6 hours and lasts for about a day.
A parasympathomimetic drug, sometimes called a cholinomimetic drug or cholinergic receptor stimulating agent, is a substance that stimulates the parasympathetic nervous system (PSNS). These chemicals are also called cholinergic drugs because acetylcholine (ACh) is the neurotransmitter used by the PSNS. Chemicals in this family can act either directly by stimulating the nicotinic or muscarinic receptors, or indirectly by inhibiting cholinesterase, promoting acetylcholine release, or other mechanisms.
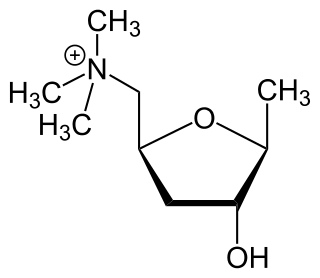
Muscarinic acetylcholine receptors, or mAChRs, are acetylcholine receptors that form G protein-coupled receptor complexes in the cell membranes of certain neurons and other cells. They play several roles, including acting as the main end-receptor stimulated by acetylcholine released from postganglionic fibers in the parasympathetic nervous system.

Galantamine,, is used for the treatment of cognitive decline in mild to moderate Alzheimer's disease and various other memory impairments. It is an alkaloid that has been isolated from the bulbs and flowers of Galanthus nivalis, Galanthus caucasicus, Galanthus woronowii, and some other members of the family Amaryllidaceae, such as Narcissus (daffodil), Leucojum aestivum (snowflake), and Lycoris including Lycoris radiata. It can also be produced synthetically.

Deliriants are a class of hallucinogen. The term was introduced by David F. Duncan and Robert S. Gold to distinguish these drugs from psychedelics and dissociatives, such as LSD and ketamine respectively, due to their primary effect of causing delirium, as opposed to the more lucid states produced by such other hallucinogens as those represented by psychedelics and dissociatives. The term is generally used to refer to anticholinergic drugs which are substances that inhibit the function of the neurotransmitter acetylcholine. Common examples of deliriants include plants of the genus Datura as well as higher than recommended dosages of Diphenhydramine (Benadryl).
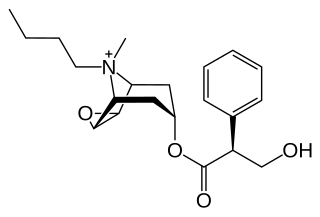
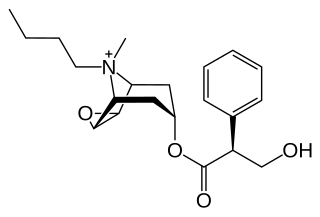
Hyoscine butylbromide, also known as scopolamine butylbromide and sold under the brandname Buscopan among others, is an anticholinergic medication used to treat crampy abdominal pain, esophageal spasms, renal colic, and bladder spasms. It is also used to improve respiratory secretions at the end of life. Hyoscine butylbromide can be taken by mouth, injection into a muscle, or into a vein.

Methacholine is a synthetic choline ester that acts as a non-selective muscarinic receptor agonist in the parasympathetic nervous system.
A cholinergic crisis is an over-stimulation at a neuromuscular junction due to an excess of acetylcholine (ACh), as a result of the inactivity of the AChE enzyme, which normally breaks down acetylcholine.

Oxybutynin, sold as under the brand names Ditropan among others, is a medication used to treat overactive bladder. It works similar to tolterodine. While used for bed wetting in children, evidence to support this use is poor. It is taken by mouth or applied to the skin.
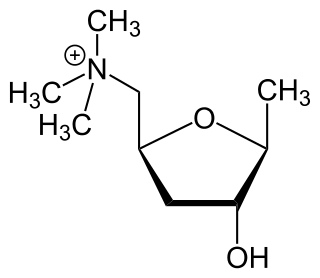
A muscarinic agonist is an agent that activates the activity of the muscarinic acetylcholine receptor. The muscarinic receptor has different subtypes, labelled M1-M5, allowing for further differentiation.

Methylscopolamine or methscopolamine, usually provided as the bromide or nitrate salt, is an oral medication used along with other medications to treat peptic ulcers by reducing stomach acid secretion. Proton pump inhibitors and antihistamine medications have made this use obsolete. It can also be used for stomach or intestinal spasms, to reduce salivation, and to treat motion sickness. Methscopolamine is also commonly used as a drying agent, to dry up post-nasal drip, in cold, irritable bowel syndrome and allergy medications
A muscarinic receptor antagonist (MRA) is a type of anticholinergic agent that blocks the activity of the muscarinic acetylcholine receptor. The muscarinic receptor is a protein involved in the transmission of signals through certain parts of the nervous system, and muscarinic receptor antagonists work to prevent this transmission from occurring. Notably, muscarinic antagonists reduce the activation of the parasympathetic nervous system. The normal function of the parasympathetic system is often summarised as "rest-and-digest", and includes slowing of the heart, an increased rate of digestion, narrowing of the airways, promotion of urination, and sexual arousal. Muscarinic antagonists counter this parasympathetic "rest-and-digest" response, and also work elsewhere in both the central and peripheral nervous systems.

Indeloxazine (INN) is an antidepressant and cerebral activator that was marketed in Japan and South Korea by Yamanouchi Pharmaceutical Co., Ltd for the treatment of psychiatric symptoms associated with cerebrovascular diseases, namely depression resulting from stroke, emotional disturbance, and avolition. It was marketed from 1988 to 1998, when it was removed from the market reportedly for lack of effectiveness.