Lassa fever, also known as Lassa hemorrhagic fever (LHF), is a type of viral hemorrhagic fever caused by the Lassa virus. Many of those infected by the virus do not develop symptoms. When symptoms occur they typically include fever, weakness, headaches, vomiting, and muscle pains. Less commonly there may be bleeding from the mouth or gastrointestinal tract. The risk of death once infected is about one percent and frequently occurs within two weeks of the onset of symptoms. Of those who survive, about a quarter have hearing loss, which improves within three months in about half of these cases.

Severe acute respiratory syndrome (SARS) is a viral respiratory disease of zoonotic origin caused by severe acute respiratory syndrome coronavirus, the first identified strain of the SARS coronavirus species severe acute respiratory syndrome–related coronavirus (SARSr-CoV). The syndrome caused the 2002–2004 SARS outbreak. Around late 2017, Chinese scientists traced the virus through the intermediary of Asian palm civets to cave-dwelling horseshoe bats in Xiyang Yi Ethnic Township, Yunnan.

Monkeypox is an infectious disease caused by the monkeypox virus that can occur in certain animals including humans. Symptoms begin with fever, headache, muscle pains, swollen lymph nodes, and feeling tired. This is followed by a rash that forms blisters and crusts over. The time from exposure to onset of symptoms is around 10 days. The duration of symptoms is typically 2 to 5 weeks.
Post-exposure prophylaxis, also known as post-exposure prevention (PEP), is any preventive medical treatment started after exposure to a pathogen in order to prevent the infection from occurring.

In public health, contact tracing is the process of identifying persons who may have come into contact with an infected person ("contacts") and subsequent collection of further information about these contacts. By tracing the contacts of infected individuals, testing them for infection, isolating or treating the infected, and tracing their contacts, public health aims to reduce infections in the population. Diseases for which contact tracing is commonly performed include tuberculosis, vaccine-preventable infections like measles, sexually transmitted infections, blood-borne infections, Ebola, some serious bacterial infections, and novel virus infections. The goals of contact tracing are:

In health care facilities, isolation represents one of several measures that can be taken to implement in infection control: the prevention of communicable diseases from being transmitted from a patient to other patients, health care workers, and visitors, or from outsiders to a particular patient. Various forms of isolation exist, in some of which contact procedures are modified, and others in which the patient is kept away from all other people. In a system devised, and periodically revised, by the U.S. Centers for Disease Control and Prevention (CDC), various levels of patient isolation comprise application of one or more formally described "precaution".

Sexually transmitted infections (STIs), also referred to as sexually transmitted diseases (STDs) and the older term venereal disease, are infections that are commonly spread by sexual activity, especially vaginal intercourse, anal sex and oral sex. STIs often do not initially cause symptoms, which results in a greater risk of passing the infection on to others. Symptoms and signs of STIs may include vaginal discharge, penile discharge, ulcers on or around the genitals, and pelvic pain. STIs can be transmitted to an infant before or during childbirth, which may result in poor outcomes for the infant. Some STIs can cause infertility.
Infectious diseases within American correctional settings are a concern within the public health sector. The corrections population is susceptible to infectious diseases through exposure to blood and other bodily fluids, drug injection, poor health care, prison overcrowding, demographics, security issues, lack of community support for rehabilitation programs, and high-risk behaviors. The spread of infectious diseases, such as HIV and other sexually transmitted diseases, hepatitis C (HCV), hepatitis B (HBV), and tuberculosis, result largely from needle-sharing, drug use, and consensual and non-consensual sex among prisoners. HIV and hepatitis C need specific attention because of the specific public health concerns and issues they raise.

Ebola, also known as Ebola virus disease (EVD) or Ebola hemorrhagic fever (EHF), is a viral hemorrhagic fever of humans and other primates caused by ebolaviruses. Signs and symptoms typically start between two days and three weeks after contracting the virus with a fever, sore throat, muscular pain, and headaches. Vomiting, diarrhoea and rash usually follow, along with decreased function of the liver and kidneys. At this time, some people begin to bleed both internally and externally. The disease has a high risk of death, killing 25% to 90% of those infected, with an average of about 50%. This is often due to shock from fluid loss, and typically follows six to 16 days after symptoms appear.

The COVID-19 pandemic, also known as the coronavirus pandemic, is an ongoing global pandemic of coronavirus disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The virus was first identified in December 2019 in Wuhan, China. The World Health Organization declared a Public Health Emergency of International Concern on 30 January 2020, and later declared a pandemic on 11 March 2020. As of 7 July 2021, more than 184 million cases have been confirmed, with more than 3.99 million confirmed deaths attributed to COVID-19, making it one of the deadliest pandemics in history.

Coronavirus disease 2019 (COVID-19) is a contagious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The first known case was identified in Wuhan, China in December 2019. The disease has since spread worldwide, leading to an ongoing pandemic.

The COVID-19 pandemic in Iceland is part of the worldwide pandemic of coronavirus disease 2019 caused by severe acute respiratory syndrome coronavirus 2. The virus was confirmed to have reached Iceland in February 2020. As of 30 June 2021, the total number of cases registered was 6,664, of which 6,604 had recovered and 30 deaths had occurred. With a total population of 368,590, the infection rate is 1 case per 61 inhabitants; the infection rate was one of the highest in the world throughout March and April, though this was attributed to more tests having been carried out per capita in Iceland than any other country, including a screening of the general population run by Icelandic biotech company deCODE genetics to determine the true spread of the virus in the community. Iceland is unique in that for each identified case of COVID-19, the genome of the virus having caused the infection is sequenced; the sequencing is carried out by deCODE genetics, which has been able to confirm that the so-called "British variant" B.1.1.7 is present in the country, whereas "South African variant" B.1.351 is not; the "Brazilian variant" B.1.1.248 is thought, but not yet confirmed, to have arrived in Iceland as of 22 March 2021.

The COVID-19 pandemic in Cambodia is part of the ongoing worldwide pandemic of coronavirus disease 2019 caused by severe acute respiratory syndrome coronavirus 2. The first imported case in Cambodia was detected in Sihanoukville on 27 January 2020. Although a number of imported cases and transmission to direct contacts were confirmed throughout 2020, no community transmission was detected until 29 November 2020.

Hazard controls for COVID-19 in workplaces are the application of occupational safety and health methodologies for hazard controls to the prevention of coronavirus disease 2019 (COVID-19). The proper hazard controls in the workplace depend on the worksite and job task, based on an occupational risk assessment of sources of exposure, disease severity in the community, and risk factors of individual workers who may be vulnerable to contracting COVID-19.

COVID-19 surveillance involves monitoring the spread of the coronavirus disease in order to establish the patterns of disease progression. The World Health Organization (WHO) recommends active surveillance, with focus of case finding, testing and contact tracing in all transmission scenarios. COVID-19 surveillance is expected to monitor epidemiological trends, rapidly detect new cases, and based on this information, provide epidemiological information to conduct risk assessment and guide disease preparedness.

COVID-19 apps are mobile software applications for digital contact tracing during the COVID-19 pandemic, i.e. the process of identifying persons ("contacts") who may have been in contact with an infected individual.
In epidemiology, a non-pharmaceutical intervention (NPI) is any method to reduce the spread of an epidemic disease without requiring pharmaceutical drug treatments. The US Centers for Disease Control and Prevention (CDC) points to Personal NPIs, Community NPIs and Environmental NPIs. NPI have been recommended for pandemic influenza at both local and global levels, and studied at large scale during the 2009 swine flu pandemic and the COVID-19 pandemic. NPIs are a set of measures that can be utilized at any time, and are used in the period between the emergence of an epidemic disease, and the deployment of an effective vaccine.
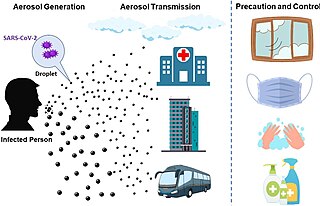
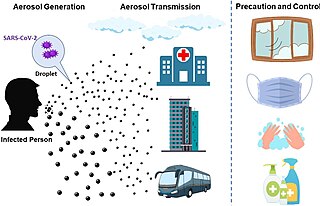
The transmission of COVID-19 is the passing of coronavirus disease 2019 from person to person. The disease is mainly transmitted via the respiratory route when people inhale droplets and particles that infected people release as they breathe, talk, cough, sneeze, or sing. Infected people are more likely to transmit COVID-19 the when they are physically close. However, infection can occur over longer distances, particularly indoors.

Speed and scale are key to mitigation of COVID-19, due to the fat-tailed nature of pandemic risk and the exponential growth of COVID-19 infections. For mitigation to be effective, (a) chains of transmission must be broken as quickly as possible through screening and containment, (b) health care must be available to provide for the needs of those infected, and (c) contingencies must be in place to allow for effective rollout of (a) and (b).

The glossary of the COVID-19 pandemic is a list of definitions of terms relating to the COVID-19 pandemic. The pandemic has created and popularized many terms relating to disease and videoconferencing.