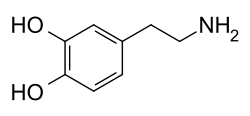
Dopaminergic means "related to dopamine" (literally, "working on dopamine"), a common neurotransmitter. [1] Dopaminergic substances or actions increase dopamine-related activity in the brain.
Contents
- Dopaminergic agents
- Dopamine precursors
- Dopamine receptor ligands
- Dopamine transporter modulators and related
- Dopamine metabolism modulators
- Dopaminergic neurotoxins
- Miscellaneous agents
- See also
- References
Dopaminergic brain pathways facilitate dopamine-related activity. For example, certain proteins such as the dopamine transporter (DAT), vesicular monoamine transporter 2 (VMAT2), and dopamine receptors can be classified as dopaminergic, and neurons that synthesize or contain dopamine and synapses with dopamine receptors in them may also be labeled as dopaminergic. Enzymes that regulate the biosynthesis or metabolism of dopamine such as aromatic L-amino acid decarboxylase or DOPA decarboxylase, monoamine oxidase (MAO), and catechol O-methyl transferase (COMT) may be referred to as dopaminergic as well.
Also, any endogenous or exogenous chemical substance that acts to affect dopamine receptors or dopamine release through indirect actions (for example, on neurons that synapse onto neurons that release dopamine or express dopamine receptors) can also be said to have dopaminergic effects, two prominent examples being opioids, which enhance dopamine release indirectly in the reward pathways, and some substituted amphetamines, which enhance dopamine release directly by binding to and inhibiting VMAT2.